RARE DISEASES IN THE MIDST OF A PANDEMIC: Silver Linings for Tomorrow?
Numerous studies and clinical trials are ongoing for Covid-19, the global pandemic that is raging through our country and the rest of the world. More than one-thousand[1], to be exact. Existing treatments for other diseases are already being repurposed—tested and used against the deadly virus in on-going trials. A novel vaccine is already being tested on humans—not mice, or rats, or monkeys, but humans. A hoped for final product is expected in the next 12-18 months. All this in just three months’ time. And while many critics wait impatiently, frustrated that cures can’t be developed more quickly, those of us in the rare disease world have stood, mouths agape, incredulous at the speed at which therapeutics are moving.
What most people don’t know is that drugs, treatments, vaccines, and cures of all kinds typically take a decade or more to make it from the lab to humans. The rare disease world is a place where we have seen this timeline occasionally upended, but only if all of the pieces that go into drug development—research, funding, regulatory pathways, urgency, and sharing of scientific information--somehow come together in a perfect synchronous wave.
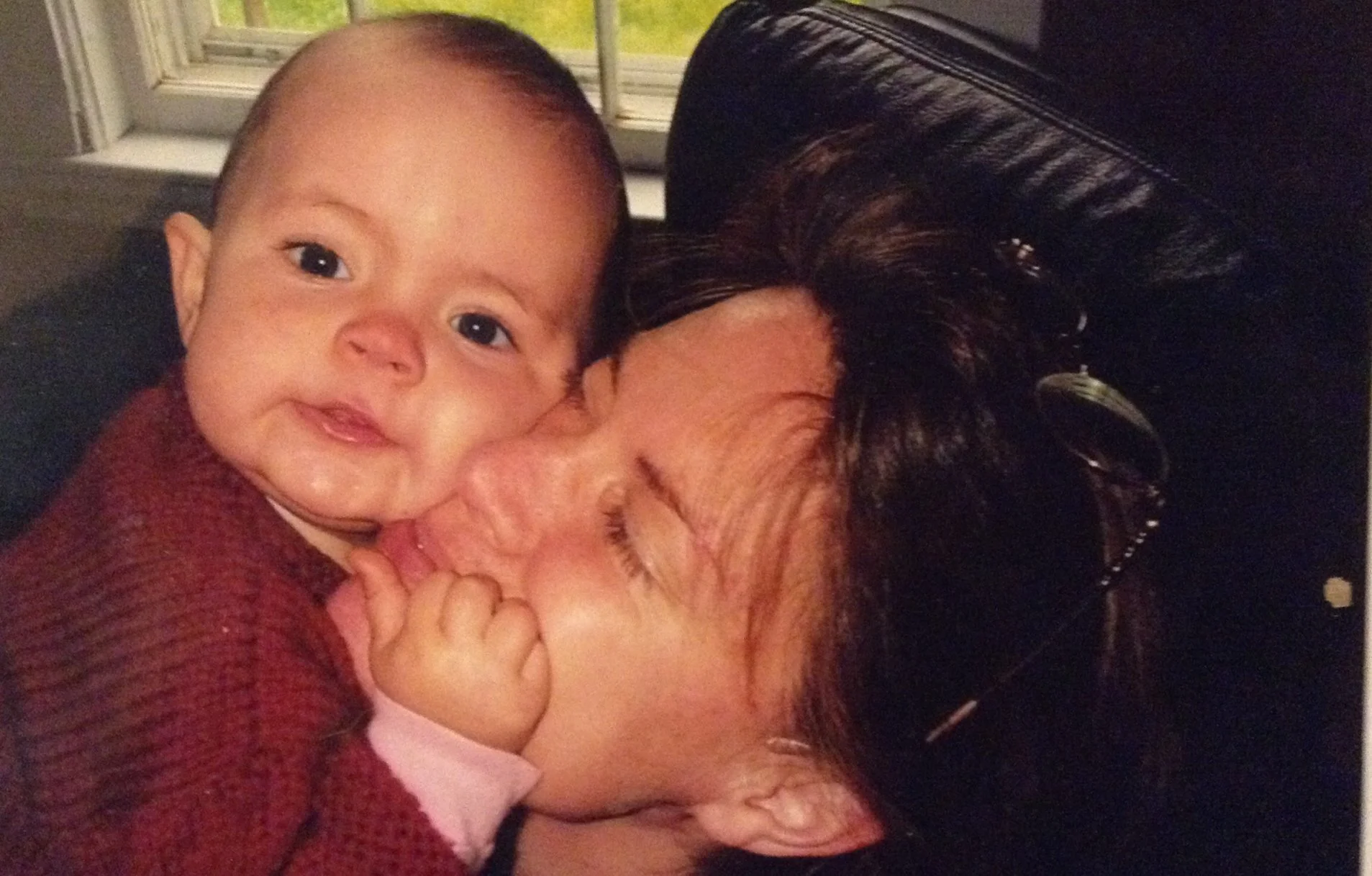
When we started the fight to save our daughter’s life, nearly four years ago, spearheading research and funding for her rare disease—Charcot Marie Tooth disease type 4J (CMT4J), a disease very much like ALS, I was assured that our science was straightforward. A deadly disease that could be cured by giving back the gene it was missing, we already knew that too much gene was okay, too. CMT4J mouse models treated with gene therapy were living out normal lifespans compared with their untreated counterparts who died in just a few weeks.
Eager, well-meaning researchers offered hopeful, but supposedly realistic timelines of eighteen months to a clinical trial—similar to what we’re hoping for with the Covid vaccine, but virtually unheard of in the larger world of translational research, and typically not for a rare disease. When we had early proof of concept using gene therapy—signs that our treatment was working in mice—I thought we just might make it. Talia had already lost so much, but I held out hope that gene therapy could halt further progression and possibly even reverse some of CMT4J’s horrific effects in her and others with her disease.
Now, nearly four years later, I am dumbfounded as I look back on our original timelines and cost estimates. In the last four years Talia has gone from walking, to walker, to wheelchair. Her arms—once a way for her to express the buckets of joy that overflow and emanate, like an endless ripple effect, from her being—now hang limply at her side. Her breath and voice have been stolen, silently over the years, leaving her dependent on a sip-ventilator during the day and a bipap machine that breathes for her at night.
A halo of cornsilk-colored hair encircles her sweet, sleepy face as I enter her room each morning to begin the daily cycles of breathing treatments. She smiles up at me, behind her bipap mask, as she waits for it to be replaced with a single straw that gives her life while awake. Over the years she has adapted from one heartbreaking loss to the next. An infinite supply of resilience and a certain amount of eagerness to live life enough to show anyone the magnitude of love and lightness she has to offer, to bother her sister just enough to make it all real, to teach all of us an ounce of empathy.
What would her life look like now? If only we had been able to treat her back then.
The race to save Talia and others has become an endless, heartbreaking slog. Regulatory guidelines change constantly, driven by the never-ending quest for more and more knowledge and the need for safety beyond any ounce of doubt. We are stuck in a process meant for drug development for more common diseases, with little regard for risk vs. benefit in deadly diseases like Talia’s.
We need a treatment now. We needed a treatment four years ago.
And as we worked our way from a first meeting of scientific investigators, through proof of concept, onward to our first FDA meeting, the cost of a gene therapy trial inched ever upward. As more and more people pursued treatments and cures with gene therapy, the supply and demand cycle responded in kind. Estimated costs of getting through a phase 1 trial inexplicably rose from $2 million to more than $5 million in just over two years.
Like so many of my rare disease colleagues, I fear I will become yet another parent whose child is deemed too far advanced in disease to become part of a clinical trial--or worse, the next one to lose her child before a treatment or cure can be realized.
Given the swift reaction of scientists, philanthropists, and government in the face of Covid-19, it is obvious that research does not have to progress this slowly. Allied against a common enemy, researchers are working cooperatively, sharing information rather than competing in silos. Redundant or unnecessary pre-clinical studies and animal testing are being waived. Regulatory guidelines and restrictions have been pushed aside to make way for a speedier path to a treatment.
I understand that a global pandemic fighting an unpredictable, deadly virus demands far greater attention than an ultra-rare disease. But I also know the other numbers—the fact that rare diseases affect nearly 400 million people worldwide. That 50% of these diseases affect children. That half of those will die before the age of five. That 95% of rare diseases still have NO known treatment or cure. And that most of the treatments for these rare diseases are being driven by the very parents and patients affected by them.
I am unaware of any annual death rate statistics for the rare disease population, but suppose we postulated that approximately 1% of people with a rare disease die each year as a result of their disease. This seems a conservative estimate. This would mean that 4 million people die every year due to rare disease. Every single year. A large proportion of these deaths are children. If this were a pandemic causing this magnitude of devastation, the world would come together to address how to stop it.
A separate, but vital conversation revolves around the cost of treating the cumulative effects of these rare, chronic, often progressive diseases—the billions of dollars that could be saved in hospitalizations, medical equipment and therapies if we could develop meaningful treatments and cures to prevent the devastating effects of these diseases.
Could the sheer recognition that research can move faster and more efficiently, become a silver lining to come out of a devastating global pandemic?
Scientists, FDA, pharma, biotech and the entities that fund them all realized quickly that outdated regulations and pathways set up decades ago for common diseases and far less urgent drug development needed to be pushed aside. Aren’t the effects of many rare diseases—a progressive and deadly course—similar to Covid-19’s worst cases? Can’t we—shouldn’t we--use this same model to address expediting treatments for rare diseases?
We actually have an existing model, in Milasen[2]*, where a drug designed to save the life of one girl was approached with a similar level of urgency, dedication and expertise as Covid-19. In less than a year Mila’s deadly form of Batten Disease was pushed from diagnosis to treatment because the stars aligned, from the science in the lab to a driven parent who succeeded in fundraising and conveying the urgency of her mission to researchers and FDA. But more importantly, Mila’s treatment moved so quickly because it was viewed as a treatment—a lifesaving drug--not a pathway for drug development.
Could a task force challenged with the expedition of rare disease treatments be modeled after Milasen and Covid-19?
Like everyone, the rare disease community has lost so much already during the Covid-19 pandemic: lives of real people who contributed to society in a myriad of ways; civil rights in a heated debate over who gets lifesaving care when hospitals are overwhelmed; individualized therapies and schooling; and research for nearly every area of medicine and health care not related to Covid-19 has come to a grinding halt.
As I write this, gene therapy is being looked at as another approach toward a vaccine for Covid-19. All eyes of the rare disease world are focused on this development, since gene therapy is a hoped-for holy grail for many single-gene rare diseases.
If we can get over a thousand studies and trials up and running in three months' time, openly share scientific discovery, rewrite ill-fitting guidelines and rules, and coordinate funding efforts between the public and private sector, then perhaps we can achieve a small percentage of this same effort for rare diseases.
Millions of lives are lost to rare diseases—an amount on par with a global pandemic. Every single year.
[1] https://clinicaltrials.gov/ct2/results?cond=Covid-19&term=&cntry=&state=&city=&dist=
[2] The New England Journal of Medicine. “Patient-Customized Oligonucleotide Therapy for A Rare Genetic Disease. https://www.nejm.org/doi/full/10.1056/NEJMoa1813279